Cancer care is evolving rapidly, and Dr. Mohan Menon, a renowned medical oncologist in Mumbai, is at the forefront of this transformation. Immune checkpoint inhibitors, including PD-1 and PD-L1 inhibitors have redefined cancer treatment by empowering the immune system to target and destroy cancer cells effectively.
This guide explores how these innovative therapies work, the cancers they treat, their benefits, side effects, and future possibilities, showcasing why immune checkpoint inhibitor immunotherapy is reshaping the fight against cancer.
Read on to understand how these cutting-edge therapies are changing lives.
What Are PD-1 and PD-L1 Inhibitors?
PD-1 and PD-L1 inhibitors are revolutionary cancer treatments that fall under a category called immunotherapy. Unlike traditional cancer therapies such as chemotherapy and radiation, these medicines work by enhancing your body’s natural defense system to fight cancer.
The immune system is your body’s built-in defense mechanism that identifies and eliminates harmful invaders like bacteria, viruses, and even cancer cells. However, some cancer cells develop clever ways to hide from the immune system, allowing them to grow and spread unchecked. PD-1 and PD-L1 inhibitors stop cancer cells from using these tricks, giving your immune system the tools it needs to attack and destroy them.
Dr. Menon explains that this approach is particularly groundbreaking because it targets cancer indirectly, by unleashing the power of your own immune system. For many patients, this means fewer side effects, longer-lasting results, and improved quality of life compared to traditional treatments.
What Are PD-1 and PD-L1?
To understand how these medicines work, it helps to know a little about PD-1 and PD-L1. PD-1, or Programmed Death-1, is a protein found on immune cells called T-cells.
“Think of PD-1 as a brake on your immune system—it prevents T-cells from attacking normal, healthy cells in your body. This is an important function because it keeps your immune system from going overboard and causing damage to healthy tissues,” states Dr. Mohan Menon, an expert medical oncologist in Mumbai.
PD-L1, or Programmed Death-Ligand 1, is a protein found in some cells, including cancer cells. “It works like a key that fits into the PD-1 “lock” on T-cells. When PD-L1 binds to PD-1, it tells the T-cell to back off and stop attacking,” he adds.
Cancer cells often produce large amounts of PD-L1 to take advantage of this system. By tricking T-cells into thinking they are harmless, cancer cells can grow and spread without interference from the immune system.
How Do PD-1 and PD-L1 Inhibitors Work?
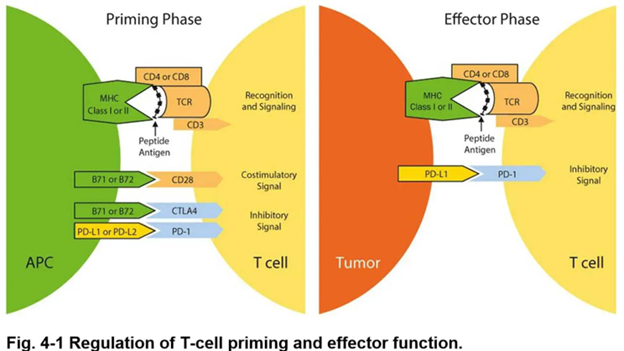
PD-1 and PD-L1 inhibitors are drugs designed to block the connection between these two proteins. Imagine that PD-L1 is the key cancer cells use to lock the immune system. These inhibitors take the key away, preventing the cancer cells from “locking out” the T-cells.
Once the PD-1/PD-L1 connection is blocked, T-cells can recognize cancer cells as harmful and launch an attack against them. This enables the immune system to do what it was meant to do—destroy cancer cells.
There are two main types of these inhibitors:
- PD-1 inhibitors, like pembrolizumab (Keytruda) and nivolumab (Opdivo), target the PD-1 protein in T-cells.
- PD-L1 inhibitors, like atezolizumab (Tecentriq) and durvalumab (Imfinzi), target the PD-L1 protein on cancer cells.
These immune checkpoint inhibitors can be used alone or in combination with other therapies, depending on the type and stage of cancer.
Does immune checkpoint inhibitor immunotherapy give you hope? Consult a medical oncologist to see if it’s right for you.
Which Cancers Can Be Treated with These Medicines?
PD-1 and PD-L1 inhibitors have been approved to treat a wide variety of cancers. They are particularly effective in cancers where the tumor cells have high levels of PD-L1. Some of the cancers treated with these medicines include:
- Lung cancer, especially non-small cell lung cancer (NSCLC), is one of the most common cancers treated with PD-1 and PD-L1 inhibitors. These drugs are often used when traditional treatments like chemotherapy are not effective or as a first-line therapy in cases with high PD-L1 levels.
- Melanoma, a dangerous form of skin cancer, has seen dramatic improvements in survival rates thanks to these inhibitors.
- Kidney cancer, or renal cell carcinoma, responds well to these drugs, especially when combined with other treatments.
- Head and neck cancers, including squamous cell carcinomas, are often treated with PD-1 inhibitors in advanced stages.
- Triple-negative breast cancer, an aggressive type of breast cancer, can be treated with PD-L1 inhibitors in some cases.
- Other cancers, such as bladder cancer, Hodgkin lymphoma, and certain rare types like Merkel cell carcinoma, have also shown good responses to these therapies.
While these drugs have brought hope to many, it’s important to note that not all patients will benefit from them. Factors like cancer type, stage, and individual health conditions play a role in determining their effectiveness.
What Are the Benefits of Immune Checkpoint Inhibitors?
One major advantage is that these treatments can lead to long-lasting responses. In some cases, patients have remained cancer-free for years after stopping treatment. This is a stark contrast to chemotherapy, which often needs to be repeated to keep cancer under control.
Another benefit is that these inhibitors specifically target the immune system, sparing healthy cells from damage. This makes them more precise than traditional treatments like chemotherapy and radiation, which can harm healthy tissues along with cancer cells.
Patients also report fewer side effects with these drugs. While there can still be side effects, they are often less severe than those caused by chemotherapy, leading to a better quality of life during treatment.
Are There Any Side Effects?
Like all medicines, PD-1 and PD-L1 inhibitors can cause side effects. Most of these happen because the immune system becomes more active and may attack healthy cells by mistake. Common side effects include:

Fatigue, which is the most frequently reported issue.
Skin problems like rashes or itching.
Diarrhea or other stomach issues caused by inflammation in the digestive system.
Pneumonitis, which is inflammation of the lungs and can cause shortness of breath or coughing.
Hormonal changes, such as thyroid problems, due to inflammation in glands that produce hormones.
These side effects can usually be managed if caught early, so it’s important to let your doctor know about any new symptoms you experience during treatment.
What Are the Challenges?
While these treatments have been revolutionary, they’re not without challenges.
Not all patients respond to PD-1 and PD-L1 inhibitors. Some cancers don’t rely on the PD-1/PD-L1 pathway to hide from the immune system, so these drugs won’t be effective.
Even when patients do respond, some cancers can develop resistance to the treatment over time. This means that after an initial period of success, the cancer may start growing again.
Another challenge is the cost of these therapies. They are expensive, which can make them inaccessible to some patients, even in countries with advanced healthcare systems.
What’s Next for These Treatments?
The field of immunotherapy is evolving rapidly, with new advances aimed at overcoming these challenges.
One exciting area is combination therapy, where PD-1 and PD-L1 inhibitors are used alongside other treatments like chemotherapy, radiation, or targeted therapies. These combinations have shown promising results in improving outcomes.
Researchers are also exploring new biomarkers to identify which patients are most likely to benefit from these treatments. By tailoring therapies to individual patients, doctors hope to make these treatments more effective.
Finally, scientists are investigating other immune pathways that cancer cells use to evade the immune system. New drugs targeting these pathways may complement PD-1 and PD-L1 inhibitors, providing even more options for patients.
Final Thoughts
PD-1 and PD-L1 inhibitors have transformed cancer treatment, offering new hope to patients around the world. While they are not a cure, they have significantly improved survival rates and quality of life for many. The future of cancer treatment looks brighter than ever, thanks to ongoing research and innovation in this field.
If you’re interested in learning more or finding out if these treatments are right for you, speak with your doctor or a cancer specialist. Staying informed and proactive can make all the difference.
Stay Informed
Subscribe to our updates or book an appointment to explore how these treatments could benefit you or your loved ones.
Frequently Asked Questions
Do immune checkpoint inhibitors guarantee a cure?
How soon can I expect to see results from immune checkpoint inhibitors?
What happens if my cancer doesn’t respond to immune checkpoint inhibitors?
Can immune checkpoint inhibitors be used as a first-line treatment?
Are immune checkpoint inhibitors effective for cancers without PD-L1 expression?
Disclaimer: The information shared in this content is for educational purposes only and not for promotional use.

